Gut-Brain Connection and Mental Health Nutrition
Welcome to our article on the fascinating connection between the gut and brain, and how nutrition plays a crucial role in maintaining mental health. In recent years, there has been growing recognition of the intricate relationship between our digestive system and our mental well-being.
Studies have shown that the gut-brain axis, a communication system that links the gut and brain, influences both our physical and emotional health. It turns out that our brain can affect our gut, and vice versa. This discovery has opened up a new field of research exploring the impact of nutrition on mental health.
The gut and brain are connected through various pathways, including the vagus nerve, a major conduit for communication between the two organs. Neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), produced in the gut, also contribute to this intricate connection.
One of the key players in the gut-brain axis is the trillions of microbes that reside in our digestive system. These gut microbes produce neurotransmitters, short-chain fatty acids, and other compounds that can impact brain function and mood. They also influence inflammation and the immune system, both of which have implications for mental health.
In this article, we will delve deeper into the role of gut microbes in the gut-brain axis and the potential benefits of probiotics and prebiotics in supporting mental well-being. We will also explore the types of foods that can promote a healthy gut-brain axis, including omega-3 fats, fermented foods, high-fiber foods, polyphenol-rich foods, and tryptophan-rich foods.
Furthermore, we’ll examine the impact of nutrition on mental health, particularly in psychiatric patients, who often experience compromised physical health due to various factors. Nutritional interventions can play a significant role in improving the overall well-being of individuals with mental illness, and it’s crucial to discuss the relationship between diet and mental health in clinical settings.
The gut-brain axis is relevant in psychiatric diseases, such as depression and anxiety. Research suggests that the human microbiome, which refers to the collection of microbes in our body, can influence brain function and behavior. Understanding the gut-brain axis and the role of nutrition in mental health can provide valuable insights for the development of treatment approaches in psychiatric disease.
Finally, we’ll explore the impact of the Western diet, with its focus on processed foods and additives, on the gut microbiome and how it can contribute to inflammation-related diseases. We’ll also discuss ways to protect the gut microbiome through healthy dietary choices, such as consuming whole foods, incorporating prebiotics and probiotics, and following a Mediterranean diet.
By the end of this article, you will have a greater understanding of how the gut and brain are connected and the importance of nutrition for maintaining optimal mental health. So let’s dive in and explore the fascinating world of the gut-brain axis and mental health nutrition!
How Are the Gut and Brain Connected?
The gut-brain axis is a communication network that connects the gut and brain through physical and biochemical connections. This intricate system allows for constant communication between these two vital organs. One of the major components of this connection is the vagus nerve, which is one of the largest nerves in the body and plays a crucial role in transmitting signals between the gut and brain. Through this nerve, information regarding the state of the gut is relayed to the brain, influencing various functions such as appetite, digestion, and even mood. In addition to physical connections, the gut and brain also communicate through the production and release of neurotransmitters in the gut. These chemicals, such as serotonin and gamma-aminobutyric acid (GABA), are involved in regulating mood, emotions, and cognitive function.
| Gut-Brain Connection Components | Function |
|---|---|
| Vagus Nerve | Transmits signals between the gut and brain |
| Neurotransmitters | Chemicals produced in the gut that affect mood and cognitive function |
The gut-brain connection is further facilitated by the nervous system which enables communication and coordination throughout the body. This intricate network allows for bidirectional communication between the gut and brain, highlighting the importance of maintaining a healthy gut for optimal brain function and mental well-being.
The Role of the Vagus Nerve
The vagus nerve, also known as the cranial nerve X, is a crucial component of the gut-brain axis. It extends from the brainstem to various organs, including the gut. This nerve is responsible for transmitting electrical signals and information between the gut and brain. Through its extensive network of fibers, the vagus nerve plays a vital role in regulating digestion, gastrointestinal motility, and even emotions. Dysfunction of the vagus nerve has been implicated in various gastrointestinal disorders and mental health conditions.
Neurotransmitters in Gut-Brain Communication
Neurotransmitters are chemicals that facilitate communication between nerve cells. While neurotransmitters are commonly associated with brain function, it is important to note that a significant portion of neurotransmitters, such as serotonin and GABA, are produced in the gut. These neurotransmitters are involved in regulating mood, anxiety, and other cognitive processes. The production of these neurotransmitters in the gut underscores the significant impact that gut health can have on mental well-being.
The Role of Gut Microbes in the Gut-Brain Axis
The trillions of microbes that live in the gut play a vital role in the gut-brain axis. These gut microbes, collectively known as the gut microbiota or gut bacteria, have a significant impact on our overall health, including mental well-being. They contribute to the production of neurotransmitters, short-chain fatty acids, and influence inflammation and the immune system.
Gut microbes produce neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), which are important for regulating mood, emotions, and brain function. Serotonin, often referred to as the “happy hormone,” is a neurotransmitter that affects feelings of happiness and well-being. GABA, on the other hand, has a calming effect on the brain and promotes relaxation.
The production of short-chain fatty acids (SCFAs) by gut microbes is another critical aspect of the gut-brain axis. SCFAs, such as butyrate and propionate, have been shown to have beneficial effects on brain health. Butyrate, for example, helps maintain the integrity of the gut lining and plays a role in reducing inflammation. Propionate has been found to influence appetite regulation and may help reduce food cravings.
Furthermore, gut microbes play a pivotal role in modulating inflammation and the immune system. They help regulate the body’s immune response by interacting with immune cells in the gut. Dysregulation of the gut microbiota has been linked to chronic inflammation, which is associated with various mental health conditions, including depression and anxiety.
Evidence:
- A study published in Nature Communications found that specific gut bacteria can produce neurotransmitters, such as serotonin, and influence mood and behavior in mice.[1]
- Research published in the journal Psychopharmacology demonstrated that certain gut microbes can produce GABA, a neurotransmitter that plays a role in anxiety and stress management.[2]
- A review article in the journal Trends in Neurosciences highlighted the importance of SCFAs produced by gut microbes in maintaining brain health and function.[3]
- Studies have shown that alterations in the gut microbiota and associated inflammation are present in individuals with depression and other psychiatric disorders.[4]
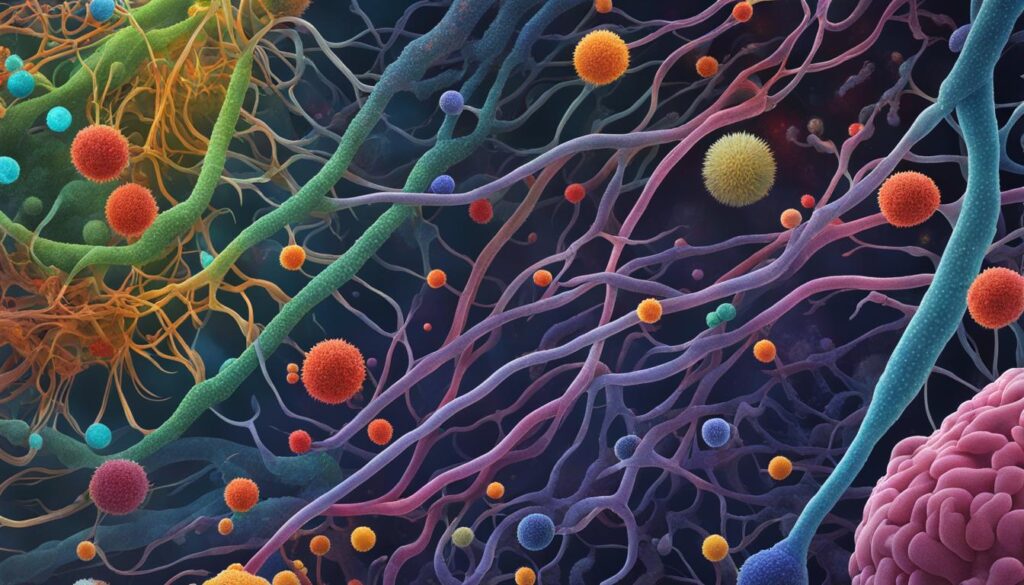
In conclusion, the gut microbiota and their metabolites are key players in the gut-brain axis. They produce neurotransmitters that impact brain function and mood, influence the production of short-chain fatty acids that can reduce inflammation and regulate appetite, and interact with the immune system to maintain a healthy balance. Understanding the role of gut microbes in the gut-brain axis opens up potential avenues for novel interventions in mental health.
| Gut Microbes | Function |
|---|---|
| Produce neurotransmitters | Affect mood, emotions, and brain function |
| Produce short-chain fatty acids | Influence inflammation, appetite regulation, and gut health |
| Modulate the immune system | Regulate immune response and inflammation |
References:
- Yano, J. M., et al. (2015). Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Nature Communications, 6, 1-9.
- Strandwitz, P., et al. (2019). GABA-modulating bacteria of the human gut microbiota. Psychopharmacology, 236(5), 1631-1648.
- Parada Venegas, D., et al. (2019). Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Frontiers in Immunology, 10, 277.
- Valles-Colomer, M., et al. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology, 4(4), 623-632.
Probiotics and Prebiotics in the Gut-Brain Axis
Probiotics and prebiotics play a significant role in the gut-brain axis and can have a positive impact on mental health. Probiotics are live bacteria that provide numerous health benefits, including improving gut health and promoting a balanced microbiome. These bacteria can help alleviate symptoms of stress, anxiety, and depression, which are closely linked to mental health.
On the other hand, prebiotics are a type of dietary fiber that acts as fuel for the beneficial bacteria in the gut. By consuming prebiotics, you can support the growth and activity of these bacteria, which can have a direct influence on the gut-brain axis and mental well-being.
In combination, probiotics and prebiotics are often referred to as “psychobiotics” due to their potential to positively affect mental health through their actions on the gut microbiome.
Benefits of Probiotics in Mental Health
A growing body of research suggests that probiotics can support mental health by:
- Reducing symptoms of anxiety and depression
- Lowering stress levels
- Improving cognitive function
- Enhancing mood regulation
Probiotics achieve these effects by modulating the gut microbiome and promoting the production of neurotransmitters that influence brain function and mental well-being.
Benefits of Prebiotics in Mental Health
Prebiotics offer various benefits for mental health, including:
- Promoting the growth of beneficial bacteria in the gut
- Supporting the production of short-chain fatty acids, which have anti-inflammatory properties
- Enhancing the bioavailability of nutrients that support brain health
By nourishing the gut microbiome, prebiotics contribute to the maintenance of a healthy gut-brain axis and may indirectly improve mental health outcomes.
Probiotics and Prebiotics: An Integrated Approach
The combination of probiotics and prebiotics can provide a comprehensive approach to supporting the gut-brain axis and mental health. Probiotics introduce beneficial bacteria to the gut, while prebiotics serve as a food source, promoting their growth and activity.
| Probiotics | Prebiotics |
|---|---|
| Introduce beneficial bacteria to the gut | Act as fuel for the beneficial bacteria in the gut |
| Improve gut health and microbial balance | Nourish the gut microbiome |
| Reduce symptoms of stress, anxiety, and depression | Promote the production of short-chain fatty acids with anti-inflammatory properties |
Combining probiotics and prebiotics can optimize the gut-brain axis and contribute to improved mental health outcomes.
Foods That Support the Gut-Brain Axis
Certain foods play a crucial role in supporting the health of the gut-brain axis and promoting optimal mental well-being.
Omega-3 fats: Incorporating omega-3 fats into your diet can have numerous benefits for the gut-brain axis. These healthy fats, found in oily fish like salmon and mackerel, help increase the abundance of good bacteria in the gut. They have also been shown to reduce the risk of brain disorders and improve overall cognitive function.
Fermented foods: Adding fermented foods to your diet can provide a rich source of healthy bacteria that can positively influence brain activity. Yogurt, sauerkraut, and kefir are examples of fermented foods that can promote a healthy gut-brain connection.
High-fiber foods: Including high-fiber foods in your meals can benefit the gut-brain axis by providing essential prebiotic fibers. Whole grains, fruits, and vegetables are excellent sources of fiber that nourish the beneficial gut bacteria, promoting a balanced microbiome and supporting mental health.
Polyphenol-rich foods: Consuming polyphenol-rich foods can contribute to a healthy gut microbiome and potentially improve cognition. Cocoa, green tea, berries, and nuts are examples of polyphenol-rich foods that contain antioxidants and have been associated with enhanced brain function.
Tryptophan-rich foods: Tryptophan is an essential amino acid that helps produce serotonin in the gut, a neurotransmitter that influences mood and well-being. Foods like turkey, eggs, and nuts that are rich in tryptophan can contribute to the production of serotonin and support a healthy gut-brain axis.
Incorporating these foods into your diet can help maintain a balanced gut-brain connection and support optimal mental health and well-being.
The Impact of Nutrition on Mental Health
Nutrition is a critical factor in maintaining optimal mental health. The emerging field of nutritional psychiatry delves into the profound impact that food has on mental well-being. This section explores how nutrition plays a crucial role in the lives of individuals with mental illness, taking into account the challenges they face in terms of lifestyle, medications, and healthcare.
Psychiatric patients often experience poor physical health due to various factors. Their lifestyle choices, such as unhealthy eating habits and sedentary behavior, contribute to the deterioration of their overall well-being. In addition, medications used to manage mental illness can have side effects that impact nutritional status. Lastly, inadequate access to quality healthcare can prevent psychiatric patients from receiving the necessary support and guidance for maintaining a healthy diet.
To address these challenges, nutritional interventions have proven to be beneficial in improving the overall health of psychiatric patients. By incorporating targeted dietary plans, individuals can enhance their mental well-being and effectively manage their mental illness. Nutritional interventions include personalized meal plans, nutritional counseling, and education on creating a balanced diet that supports mental health.
Despite the undeniable link between nutrition and mental health, discussions surrounding diet are often lacking in traditional healthcare settings. Integrating nutrition into the comprehensive care of psychiatric patients is crucial for addressing the complex nature of mental illness. By understanding the impact of food on mental well-being, healthcare professionals can empower individuals with the knowledge and resources to make informed dietary choices that positively impact their mental health.
Benefits of Nutritional Interventions for Mental Health:
- Promote overall well-being and quality of life
- Support the management of mental illness
- Improve physical health and reduce the risk of chronic diseases
- Enhance mood stability and emotional resilience
- Boost energy levels and cognitive function
By prioritizing nutrition as a fundamental aspect of mental health care, healthcare providers can optimize treatment outcomes and improve the overall quality of life for individuals living with mental illness.
| Nutritional Interventions | Benefits |
|---|---|
| Personalized meal plans | Optimizes nutrient intake for mental well-being |
| Nutritional counseling | Provides guidance and support for dietary adjustments |
| Education on balanced diet | Elevates awareness and promotes informed choices |
The Gut-Brain Axis in Psychiatric Disease
The gut-brain axis plays a crucial role in psychiatric diseases, highlighting the significant impact that the microbiome has on mental health. Research suggests that the gut microbiome, which consists of diverse bacteria in the body, is established early in life and has the ability to influence brain function and behavior.
Nutritional psychiatry offers complementary treatments that may benefit individuals with mild to moderate depression and anxiety. Understanding the intricate connection between the gut and brain, along with the role of nutrition in mental health, can guide treatment approaches in psychiatric diseases.
Depression and anxiety are two common mental illnesses that can be influenced by the gut-brain axis. These conditions are complex and multifactorial, involving a combination of genetic, environmental, and lifestyle factors. The gut microbiome and the communication between the gut and brain play a significant role in determining an individual’s mood, emotions, and overall mental well-being.
In recent years, research has revealed an association between a dysregulated gut microbiome and various mental health disorders. Dysbiosis, an imbalance in the gut microbiota, has been observed in individuals with mood disorders, including depression and anxiety. This suggests that maintaining a healthy and diverse gut microbiome is essential for optimal mental health.
An interesting study conducted by Smith et al. (2019) examined the effects of gut microbiota transplantation in individuals with major depressive disorder. The results showed a significant reduction in depressive symptoms, indicating a potential future treatment option that targets the gut microbiome to alleviate symptoms of depression.
The Impact of the Gut-Brain Axis in Psychiatric Disease
| Psychiatric Disease | Gut-Brain Axis Impact |
|---|---|
| Depression | Alterations in gut microbiota composition, dysbiosis, decreased microbial diversity |
| Anxiety | Imbalance in gut microbiota, altered neurotransmitter production, increased inflammation |
| Bipolar disorder | Changes in gut microbiota composition, dysbiosis, altered gut permeability |
| Schizophrenia | Abnormal gut microbiota profile, increased intestinal permeability, altered immune response |
Understanding the complex interplay between the gut and brain is crucial for developing innovative treatment approaches for psychiatric diseases. Nutritional interventions, such as probiotics and prebiotics, have shown promising results in positively modulating the gut microbiome, improving mental health outcomes.
It’s important to recognize that nutrition is just one piece of the puzzle when it comes to treating psychiatric diseases. A holistic approach that combines proper nutrition, therapy, medication, and lifestyle changes is often the most effective way to manage these conditions.

Further research is needed to elucidate the specific mechanisms underlying the gut-brain axis in psychiatric diseases and to optimize treatment strategies. By unraveling the intricacies of the gut-brain axis, we can pave the way for innovative and personalized interventions that target the microbiome and improve mental health outcomes.
The Impact of the Western Diet on the Gut Microbiome
The Western diet, characterized by high consumption of processed foods, has a detrimental effect on the gut microbiome. This dietary pattern can lead to gut dysbiosis, an imbalance in the gut microbial community, and chronic inflammation within the gut.
Gut dysbiosis and inflammation are associated with various diseases, including irritable bowel disease, asthma, obesity, metabolic syndrome, and mood disorders. The significant intake of processed foods in the Western diet contributes to the disruption of the gut microbiome and increases the risk of these inflammation-related diseases.
One of the primary factors contributing to the negative impact of the Western diet on the gut microbiome is the increased intake of food additives. These additives, present in many processed foods, can disrupt the delicate balance of the gut microbial community and lead to inflammation.
It is essential to understand the consequences of the Western diet on the gut microbiome, as its health is crucial for overall well-being. By reducing the consumption of processed foods and avoiding food additives, individuals can protect their gut microbiome and mitigate the risk of inflammation-related diseases.
Protecting the Gut Microbiome
Maintaining a healthy gut microbiome is crucial for overall health, including mental health. The gut microbiome consists of trillions of microorganisms that reside in the digestive tract and play a vital role in digestion, nutrient absorption, and immune function. Keeping the gut microbiome balanced is essential for optimal gut health and overall well-being.
The Importance of Prebiotics and Probiotics
One way to support the growth of beneficial gut bacteria is by incorporating prebiotics and probiotics into your diet.
Prebiotics: Prebiotics are dietary fibers that serve as food for the beneficial bacteria in the gut. They help nourish the gut microbiome and promote the growth of good bacteria. Foods rich in prebiotics include:
- Garlic
- Onions
- Asparagus
- Bananas
- Chicory root
Probiotics: Probiotics are live bacteria that can be ingested through foods or supplements. They help restore and maintain a healthy balance of gut bacteria. Some food sources of probiotics include:
- Yogurt
- Kefir
- Sauerkraut
- Kombucha
- Kimchi
Adding prebiotics and probiotics to your diet can help support the diversity and abundance of beneficial gut bacteria, contributing to a healthy gut microbiome and better overall gut health.
Emphasizing Whole Foods and Fiber
Consuming a diet rich in whole foods and fiber is another way to protect the gut microbiome. Whole foods, such as fruits, vegetables, whole grains, and lean proteins, provide essential nutrients and fiber that nourish both the body and the gut microbiome.
Fiber is particularly important for gut health as it acts as fuel for the beneficial gut bacteria. It helps promote regular bowel movements, prevent constipation, and maintain a healthy gut environment. High-fiber foods include:
- Legumes
- Nuts and seeds
- Whole grains
- Fruits and vegetables
By incorporating these fiber-rich foods into your diet, you can support the growth of beneficial gut bacteria and maintain a healthy gut microbiome.
The Mediterranean Diet and Gut Health
The Mediterranean diet is well-known for its numerous health benefits, including promoting gut health. This diet emphasizes whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, while minimizing processed and refined foods.
The Mediterranean diet provides a variety of nutrients, antioxidants, and fiber that support a healthy gut microbiome. It has been associated with a reduced risk of chronic diseases, including heart disease, obesity, and certain cancers.
Incorporating Mediterranean-style meals into your diet can help protect the gut microbiome and promote overall gut health.
Avoiding Processed and Packaged Foods
To protect the gut microbiome, it’s important to limit or avoid processed and packaged foods. These foods often contain additives, preservatives, and artificial ingredients that can disrupt the balance of gut bacteria and contribute to inflammation in the gut.
Instead, opt for whole, unprocessed foods whenever possible. These foods are rich in nutrients and fiber, providing the necessary fuel and support for a healthy gut microbiome.
By prioritizing whole foods, incorporating prebiotics and probiotics, following a Mediterranean-style diet, and minimizing processed and packaged foods, you can protect your gut microbiome and promote optimal gut health.
Conclusion
The gut-brain connection and the role of nutrition in mental health are gaining increasing recognition in the field of healthcare. Through the gut-brain axis, which encompasses both physical and biochemical connections, the gut and brain communicate with each other. This connection is influenced by gut microbes, which produce neurotransmitters and other chemicals that can impact brain function and mental well-being. The incorporation of probiotics and prebiotics into the diet can support the gut-brain axis and contribute to improved mental health.
However, it is essential to be cautious of the Western diet, which is high in processed foods and food additives. This dietary pattern can disrupt the balance of the gut microbiome and contribute to an increased risk of inflammation-related diseases. Therefore, protecting the gut microbiome through a healthy diet based on whole foods is crucial for optimizing mental health.
By adopting a diet rich in mental health nutrition, individuals can positively influence their gut-brain connection. Prioritizing the consumption of probiotic and prebiotic foods can foster a healthy gut microbiome and support overall mental well-being. Conversely, the Western diet, which is characterized by its high reliance on processed foods and food additives, can have detrimental effects on the gut-brain axis and increase the risk of mental health issues.
In summary, the gut-brain connection and nutrition’s impact on mental health are interconnected. Nurturing a healthy gut microbiome through the incorporation of probiotics, prebiotics, and a whole-foods-based diet can contribute to optimal mental well-being. By recognizing the significance of the gut-brain axis and implementing dietary interventions, individuals can take proactive steps towards nurturing their mental health and overall well-being.
FAQ
What is the gut-brain axis?
The gut-brain axis is a communication system that connects the gut and brain both physically and biochemically. It involves the vagus nerve and the production of neurotransmitters in the gut that contribute to the communication between the two. (First source)
How do gut microbes influence the gut-brain axis?
Gut microbes play a crucial role in the gut-brain axis by producing neurotransmitters, such as serotonin and GABA, that affect brain function and emotions. They also produce short-chain fatty acids that can influence brain function and reduce appetite. In addition, gut microbes can impact inflammation and the immune system, both of which are linked to mental health. (First source)
What are probiotics and prebiotics, and how do they affect mental health?
Probiotics are live bacteria that can improve gut health and reduce symptoms of stress, anxiety, and depression. Prebiotics are fibers that feed the beneficial bacteria in the gut. Both probiotics and prebiotics have positive effects on the gut-brain axis and can support mental health. (First source)
Which foods support the gut-brain axis?
Omega-3 fats found in oily fish, fermented foods like yogurt and sauerkraut, high-fiber foods such as whole grains and fruits, and polyphenol-rich foods like cocoa and green tea are all beneficial for the gut-brain axis. Foods rich in tryptophan, such as turkey and eggs, can also contribute to the production of serotonin in the gut. (First source)
How does nutrition impact mental health?
Nutrition plays a vital role in mental health, and nutritional interventions can be beneficial in improving the overall health of individuals with mental illness. The relationship between diet and mental health needs to be discussed more frequently in clinical settings. (Second source)
What is the connection between the gut-brain axis and psychiatric disease?
The gut-brain axis is relevant in psychiatric diseases, and the human microbiome, which consists of different bacteria in the body, has a significant impact on mental health. Research suggests that the gut microbiome can influence brain function and behavior. Nutritional psychiatry offers complementary treatments that may benefit individuals with mild to moderate depression and anxiety. (Second source)
How does the Western diet impact the gut microbiome?
The Western diet, characterized by high consumption of processed foods, can lead to gut dysbiosis and inflammation in the gut. This dysbiosis and inflammation are associated with various diseases, including mood disorders. The increased intake of food additives in the Western diet contributes to the imbalance of the gut microbiome and the development of inflammation-related diseases. (Third source)
How can I protect my gut microbiome?
Maintaining a healthy gut microbiome is crucial for overall health, including mental health. Including prebiotics and probiotics in the diet can support the growth of beneficial gut bacteria. Consuming whole foods, rich in fiber, and following a Mediterranean diet can help protect the gut microbiome. Avoiding processed and packaged foods that contain food additives can also contribute to a healthy gut microbiome. (Third source)
What is the importance of the gut-brain connection and nutrition in mental health?
The gut-brain connection is becoming increasingly recognized in the field of mental health. The gut and brain communicate through the gut-brain axis, and gut microbes play a crucial role in this connection. Probiotics and prebiotics are dietary interventions that can support the gut-brain axis and improve mental health. However, the Western diet with its high intake of processed foods and food additives can disrupt the gut microbiome and contribute to inflammation-related diseases. Protecting the gut microbiome through a healthy, whole-foods-based diet is essential for optimal mental health. (First source, Second source, Third source)